Arthritis is a chronic degenerative disease that affects all parts of the joint: cartilage, joint membrane, ligaments, capsule, periarticular bones and surrounding muscles and ligaments.
According to European doctors, arthrosis accounts for almost 70% of all rheumatological diseases. People aged 40-60 years are most susceptible to arthrosis of the joints. This is facilitated both by the lack of movement and by prolonged overload, poor nutrition and, of course, injuries.
What's going on?
Normally, a human joint consists of 2 or more connecting bones. All working surfaces of the joint have a protective coating and are constantly lubricated with synovial fluid for the best gliding. The joint cavity itself is hermetically sealed by the joint capsule.
There are many joints in our body that are "responsible" for certain types of movements, can experience different loads and have different safety limits.
The amount of movement in a joint depends on the structure of the joint, the ligamentous apparatus that limits and strengthens the joint, and the various muscles attached to the bones by tendons.
Causes of arthrosis of the joints
Normal functioning of the joints is possible with constant self-renewal of cartilage tissue. At a young age, the rate of death of old joint cells is equal to the rate of birth of new cells. Over the years, the process of cell renewal slows down and cartilage tissue begins to thin. Synovial fluid production also decreases. As a result, the articular cartilage begins to thin and break down, leading to osteoarthritis.
In addition, there are other causes of joint arthrosis:
- increased physical activity. Arthrosis of the joints is often accompanied by excess weight. As a result of overloading, microtraumas are formed in the joints. Athletes develop joint damage due to increased loads on "unheated" joints;
- joint injuries;
- congenital or acquired deformities of the musculoskeletal system (rickets, kyphosis, scoliosis, improper fusion of bones after injuries with the appearance of limb deformities: O-shaped and X-shaped deformity of the legs).
Stages of arthrosis
Depending on the degree of destruction of cartilage tissue, different stages or degrees of arthrosis can be distinguished.
Degrees and symptoms of arthrosis
- Arthritis of the 1st degree is characterized by periodic pains in the joints, especially with increased physical activity. After rest, the pain usually goes away. The range of motion in the joint is not limited, the muscle strength in the injured limb does not change. X-rays can show minimal signs of joint damage.
- Arthrosis of the 2nd degree manifests itself with painful sensations not only with intense physical stress, but also with minor loads. Even during rest, joint pain may not go away. This degree is characterized by stiffness of movements and limited mobility in the joints. This eventually leads to muscle atrophy. An X-ray can show deformation of the joint, narrowing of the joint space and the appearance of bony growths near this space.
- Arthrosis 3rd degree - any movement causes a person severe pain. The joint pain is present even at rest. Therefore, one tries to move as little as possible so that the pain is minimal. In some cases, movement requires the use of crutches or a wheelchair. Sometimes there is fusion of the bones - ankylosis (as in ankylosing spondylitis).
In deforming arthrosis, irreversible changes occur in the cartilage tissue of the joint and its functions and structure are completely impaired. Deforming arthrosis of the joints is based on the appearance of dysfunction in the formation of hyaline cartilage and synovial fluid.
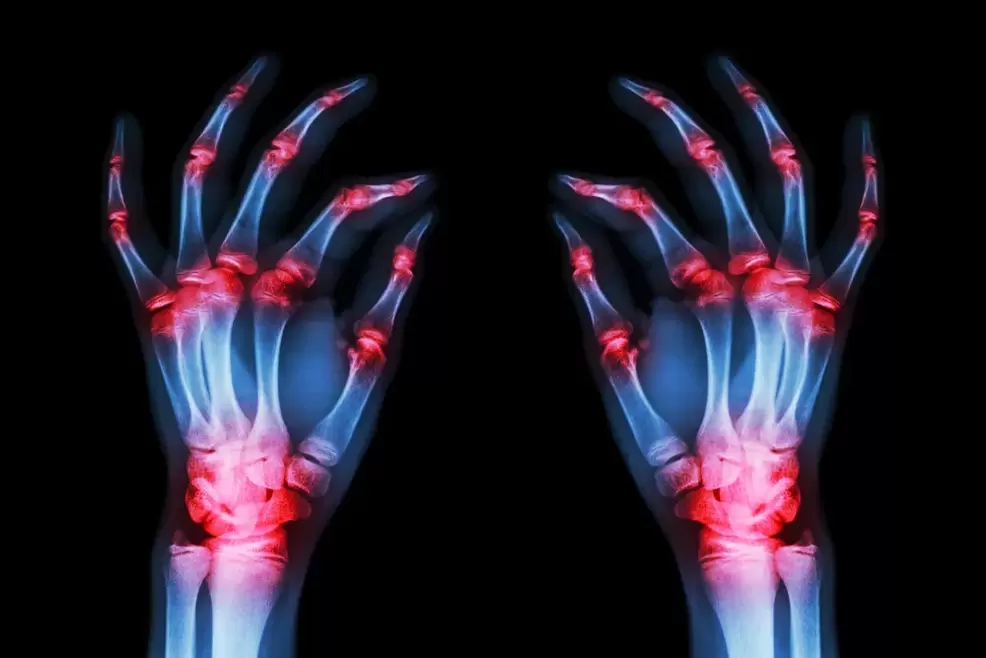
Diagnosis of joint arthrosis
The main method for diagnosing joints is radiography. With arthrosis, changes in the joints, uneven joint surfaces and narrowing of the joint space can be observed.
Which joints are more likely to suffer from osteoarthritis?
The joints of the limbs that are most susceptible to arthrosis are the hips, knees, shoulders, elbows and hands.
With arthrosis of the hip joint, a person may first feel a slight discomfort in the legs after running or walking. Over time, the pain intensifies, limitation and stiffness in movement appear. In stage 3 disease, the patient protects his foot and tries, if possible, not to step on it.
Osteoarthritis of the knee joint manifests itself as pain in the knee joint after bending and straightening the legs. The most common cause of knee osteoarthritis is past injuries. As a result of these injuries, the sliding of the joint surfaces is disturbed and their rapid wear occurs. In some cases, the joint may gradually lose its mobility.
Osteoarthritis of the ankle joint manifests itself in the form of swelling and pain in the ankle of the leg. The cause of arthrosis of the ankle joint can be: deformities, fractures of the ankles and talus, luxations, flat feet, chronic injuries of the ankle joint in athletes and ballerinas. By the way, they often have arthrosis of the foot.
Osteoarthritis of the shoulder joint, elbow and wrist most often occurs as a result of injuries, contusions, dislocations and intra-articular fractures. Osteoarthritis of the shoulder joint is characterized by pressing, aching, dull pain that radiates to the forearm and hand. Most often, the pain appears at night. In arthrosis of the hands, the pain is accompanied by dysfunction of the hand.
Treatment of arthrosis
The main means of treating arthrosis are drug treatment, use of physiotherapy and surgical treatment.
Medication treatment
The use of drugs helps to improve blood circulation in damaged joints, restore the properties of cartilage, has an analgesic and anti-inflammatory effect.
Nonsteroidal anti-inflammatory drugs
With arthrosis, swelling of the joint may occur, the joint starts to hurt and the range of motion decreases. When taking anti-inflammatory drugs (NSAIDs), the pain decreases, the inflammatory chain reaction is stopped and the cartilage repair process is accelerated.
Medicines can be used in the form of tablets, rectal suppositories and powder. But remember that self-medication is unacceptable, the choice and dosage of the drug for arthrosis is carried out by a rheumatologist.
Centrally acting pain relievers
Opioid drugs lower the patient's pain threshold. Such drugs can be taken strictly according to a doctor's prescription and only under the supervision of a doctor!
Chondroprotective drugs
Chondroprotective drugs are structural elements of the cartilage itself, therefore they actively restore this tissue and prevent its further destruction. The treatment is effective in the initial stage of the disease. When the joint is already completely destroyed, it is not possible to return the original shape of the deformed bones or to develop new cartilage.
However, at stages 1-2 of arthrosis, chondroprotectors can bring significant relief to the patient. Combined preparations, which include glucosamine and chondroitin sulfate, give better results than the single-component preparation.
Chondroitin sulfate and glucosamine sulfate
These drugs help slow the inflammatory response in the tissues, help reduce cartilage damage, and reduce pain. Most often, these 2 drugs are used together in treatment, as they have an accumulating effect, but they must be taken for 3-6 months.
Hyaluronic acid
Provides viscosity and elasticity of the synovial fluid. It helps the joints slide well. Therefore, doctors often prescribe injections of hyaluronic acid into the affected joint.
Physiotherapy procedures
Physiotherapy treatments may include:
- UHF therapy;
- magnetic therapy;
- low intensity laser irradiation;
- drug electrophoresis;
- phonophoresis (use of ultrasound to introduce medicine to the site of inflammation).
surgery
Surgical treatment is used to restore and improve the mobility of the joint, as well as to remove part of the cartilage or damaged menisci.
Surgical treatment of arthrosis is resorted to in extreme cases, when medical treatment does not give results, with severe pain, partial or complete immobility in the joints.
During arthroscopic surgery, it is possible to remove part of the cartilage affected by arthrosis, polish it to obtain a smooth surface, remove cartilage fragments and growths, and cut part of the damaged ligaments.
Knee replacement
In this operation, the articular surfaces of the knee joint are replaced with metal or combined prostheses. The prepared plates copy the surface of the articular cartilage. Such prostheses are made of special alloys, do not cause a rejection reaction in patients, do not oxidize and do not damage the surrounding tissues.
Surgery of the hip joint in arthrosis
During this operation, a partial removal of the cartilage and bone tissue of the pelvis and femur is performed. Usually, the head of the femur and the articular surface of the pelvis are removed and replaced with a metal or metal-ceramic prosthesis.
Diet for arthrosis
Excess body weight is a great enemy of your joints. Most patients suffering from arthrosis of the hip and knee joints are overweight.
That is why a properly selected diet is recommended for arthrosis. It is believed that jellied meat cooked in cartilage broth is useful for arthrosis. It contains a lot of collagen and structural components of cartilage, which help to restore cartilage tissue.
Dairy products, protein and calcium are helpful. Animal protein is found in lean meats and fish, and vegetable protein is found in buckwheat porridge, beans and lentils. Boiled, stewed and steamed dishes are very useful.
The best diet for joints is a diet with a slight predominance of carbohydrates (preferably complex carbohydrates), fruits and vegetables, and sufficient protein and calcium.
Prevention of arthrosis
The prevention of arthrosis, however trivial it may be, lies in a healthy lifestyle. If possible, try to be in the fresh air, move, walk barefoot on sand, green grass and just on the ground. This type of walking improves muscle function and increases blood circulation in the legs.
Using physical therapy with various arm and leg swings, twists and turns will provide as much support as possible for your joints.
Patients often ask if alternative treatment of arthrosis is possible? Yes, folk remedies can help in the initial stages of the disease, reduce pain and improve the general condition of the patient. But it does not replace following your doctor's instructions.



































